in case of lesions in positions at risk?
USA visitors must check the Legal Disclaimer at the end of this page

PBLite is the ECHOLASER Thermal Ablation treatment for malignant abdominal tumours, in particular primary and secondary liver cancers.
The name of the treatment encapsulates in a single word the application area (the liver, “PB” is the abbreviation of Prometheus bound, the titan who in Greek mythology was condemned to be bound to the rocks of the Caucasus while an eagle pecked at his liver each day) and “Lite”, which on one hand refers to the lightweight and micro-invasiveness of the treatment, and on the other, the therapeutic source (Light, therefore Laser).
The name PBLite marks the difference of the procedure performed with ECHOLASER (micro-invasiveness and multi-fibre approach in a single system) from the other thermal ablation techniques.
Suitability
PBLite is indicated in the treatment of primitive and secondary liver cancer in the form of focal lesions. PBLite is also a safe and effective treatment for those who, due to critical medical conditions, are unable to undergo surgery.
What is it?
PBLite consists of the percutaneous insertion of optical fibres (from 1 to 4 depending on the size of the tumour), and the delivery of laser energy for several minutes, which heats the tissues until they are completely destroyed with a sufficient safety margin. The positioning of the applicators, monitoring of the treatment and verification of the effective coagulation area are all carried out under ultrasound guidance. In order to facilitate the insertion manoeuvre, the system has dedicated multi-applicator Guiding Systems for ultrasound probes designed for the anatomical area of the liver with relative Biopsy Software that displays the guidelines on the screen. As these are malignant tumours, the objective of the treatment is a complete ablation of the lesion and subsequent absence of local post-treatment relapses and a net increase in the long-term survival probability (5 years).
With just one PBLite session it is possible to treat liver lesions with a very wide size range and diameters of up to 5 cm thanks to the versatility provided by the multi-fibre approach. The localized thermal effect of PBLite makes it the gold standard for liver lesions close to structures at risk.
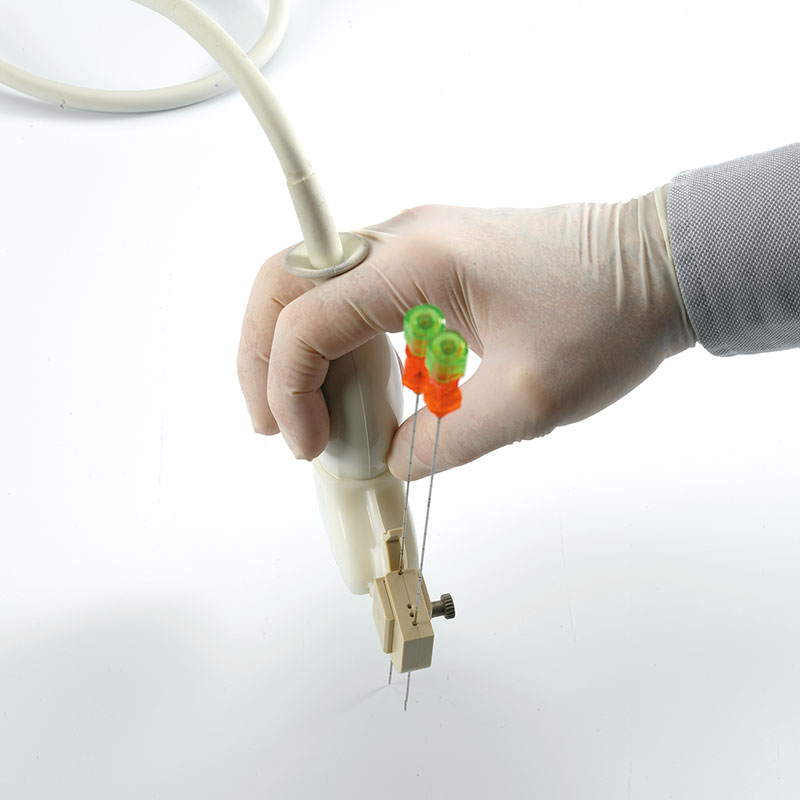
1./2. SI2C41 Esaote probe with dedicated multi-fibre Guiding System
3./4. CA541 Esaote probe with dedicated multi-fibre Guiding System
Advantages
complete ablation with a sufficient safety margin
“in situ” thermal destruction
preservation of the healthy tissue and the organ function
highly predictable and repeatable coagulation volume as required for the safety margin
localized thermal effect in the target volume only, which makes the treatment possible close to sites at risk
use of fine, non-traumatic needles for liver organ
possibility of treating patients with pace-makers (excellent electromagnetic compatibility)
no general anesthesia
short duration of the treatment (few minutes)
rapid recovery
no or insignificant post-treatment pain
brief hospitalization
bridging therapy for organ transplants
Clinical Case no.1: primary liver tumour close to vascular structures
A patient with partially exophytic liver cancer (white arrow in the Figure), located between a branch of the portal vein and the vena cava, underwent EchoLaser Thermal Ablation using four fibres, two positioned in the upper section of the portal vein and two in the lower section. The lesion which was particularly difficult to treat due to the surrounding veins, was completely ablated without any alterations to the surrounding vascular structures. 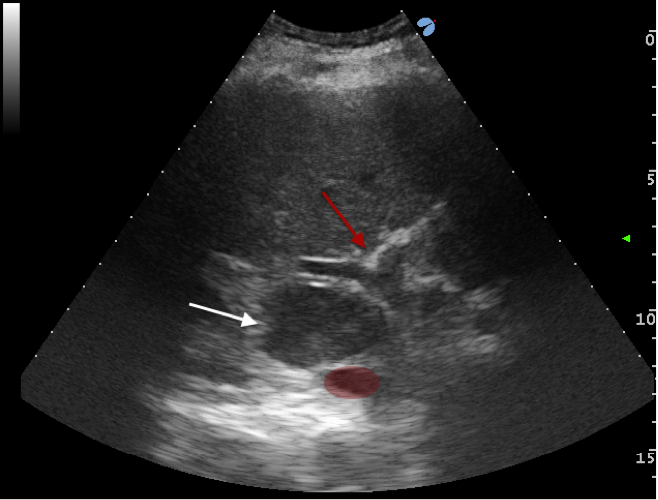
US image before the treatment 
MR image at one-month follow-up showing complete ablation (white arrow)
Images courtesy of Dr. Giovan Giuseppe Di Costanzo (Cardarelli Hospital, Naples)
Clinical Case no.2: secondary colorectal cancer close to the heart
A patient with an 8-mm metastasis of the liver in segment I extremely close to the pericardium, was subjected to the EchoLaser Thermal Ablation. The lesion was completely ablated without any complications involving critical neighbouring structures such as pericardial effusion.

US image before the treatment
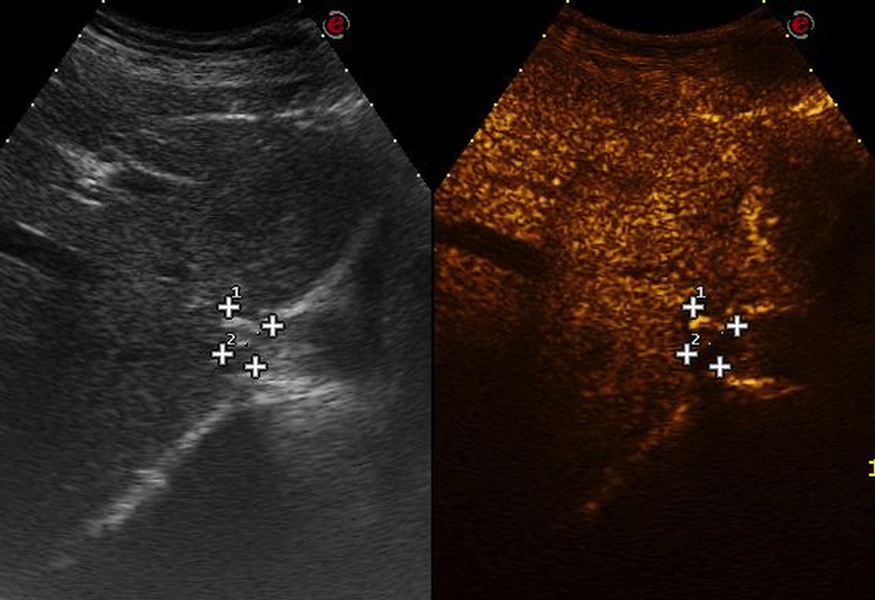
CEUS image after the treatment showing complete ablation Images courtesy of Dr. Sergio Sartori (Sant’Anna Hospital, Ferrara)
Open the following document to view other clinical cases treated with PBLite.
Percutaneous Laser Ablation of Liver Metastases from Neuroendocrine Neoplasm. A Retrospective Study for Safety and Effectiveness.
Sartori S, Tombesi P, Di Vece F, Bianchi L, Ambrosio R.
Cardiovasc Intervent Radiol. 2019 Aug 13.
Treatment response and preliminary efficacy of hepatic tumour laser ablation under the guidance of percutaneous and endoscopic ultrasonography.
Chai W, Zhao Q, Song H, Cheng C, Tian G, Jiang T.
World J Surg Oncol. 2019 Aug 5;17(1):133.
Percutaneous Laser Ablation of Hepatic Tumors Located in the Portacaval Space: Preliminary Results.
Chai W, Zhao Q, Kong D, Jiang T.
Lasers Surg Med. 2019 Jul 8.
Cost Minimization Analysis of Radiofrequency Compared to Laser Thermal Ablation in Patients with Hepatocellular Carcinoma.
Guarino M, D’Angiolella LS, Falco L, Morando F, Di Costanzo GG, Morisco F, Improta G, Mantovani LG, Caporaso N
Farmeconomia. Health economics and therapeutic pathways 2019;20(1):43-50
Laser ablation is superior to TACE in large-sized hepatocellular carcinoma: a pilot case–control study
Morisco F, Camera S, Guarino M, Tortora R, Cossiga V, Vitiello A, Cordone G, Caporaso N, Di Costanzo GG and Italian Liver Cancer (ITA.LI.CA) group
Oncotarget. 2018; 9:17483-17490.
Percutaneous Laser Thermal Ablation in a Patient with 22 Liver Metastases from Pancreatic Neuroendocrine Tumours: A Case Report
Sartori S, Di Vece F, Bianchi L, Tombesi P
EMJ Hepatol. 2018;6[1]:95-99.
EUS dating with laser ablation against the caudate lobe or left liver tumors: a win-win proposition?
Jiang T, Tian G, Bao H, Chen F, Deng Z, Li J, Chai W.
Cancer Biol Ther. 2018 Mar 4;19(3):145-152.
Efficacy and safety of percutaneous laser ablation therapy for treatment of large HCC.
Camera S, Di Costanzo GG, Tortora R, Addario L, Lampasi F, Tartaglione MT, Cossiga V, Donnaruma L, Caporaso N, Morisco F.
Digestive and Liver Disease. 2016; 48 (1): e50.
Laser ablation with or without chemoembolization for unresectable neuroendocrine liver metastases: a pilot study
Pacella CM, Nasoni S, Grimaldi F, Di Stasio E,Misischi I, Bianchetti S, Papini E.
International Journal of Endocrine Oncology May 2016, Vol.3, No.2, Pages 97-107
Laser ablation for hepatic metastases from neuroendocrine tumors
Tombesi P, Di Vece F, Sartori S.
AJR Am J Roentgenol. 2015 Jun;204(6):W732.
Laser ablation for small hepatocellular carcinoma: State of the art and future perspectives.
Di Costanzo GG, Francica G, Pacella CM.
World J Hepatol 2014 October 27; 6(10): 704-715
Radiofrequency Ablation versus Laser Ablation for the Treatment of Small Hepatocellular
Carcinoma in Cirrhosis: a Randomized Trial.
Di Costanzo GG, Tortora R, D Adamo G, De Luca M, Lampasi F, Addario L, Galeota Lanza A, Picciotto FP, Tartaglione MT, Cordone G, Imparato M, Mattera S, Pacella CM.
J Gastroenterol Hepatol. 2015 Mar;30(3): 559-65
A novel needle guide system to perform percutaneous laser ablation of liver tumors using the multifiber technique.
Di Costanzo GG, D’Adamo G, Tortora R, Zanfardino F, Mattera S, Francica G, Pacella CM.
Acta Radiol. 2013 May 23.
Effectiveness, Safety, and Local Progression After Percutaneous Laser Ablation for Hepatocellular Carcinoma Nodules up to 4 cm Are Not Affected by Tumor Location
Francica G, Petrolati A, Di Stasio E, Pacella S, Stasi R, Pacella CM.
Vascular and Interventional Radiology 2012 February;199:1393–1401
Influence of ablative margin on local tumor progression and survival in patients with HCC ≤4 cm after laser ablation.
Francica G, Petrolati A, Di Stasio E, Pacella S, Stasi R, Pacella CM.
Acta Radiol. 2012 May 1;53(4):394-400.
Percutaneous laser ablation of hepatocellular carcinoma in patients with liver cirrhosis awaiting liver transplantation
Pompili M, Pacella CM, Francica G, Angelico M, Tisone G, Craboledda P, Nicolardi E, Rapaccini GL, Gasbarrini G.
Eur J Radiol. 2009
Review Article: Laser Ablation for Small Hepatocellular Carcinoma
Pacella CM, Francica G, and Di Costanzo GG.
Radiology Research and Practise. 2011 Oct 20
Long-term outcome of cirrhotic patients with early hepatocellular carcinoma treated with ultrasound-guided percutaneous laser ablation: a retrospective analysis
Pacella CM, Francica G, Di Lascio FM, Arienti V, Antico E, Caspani B, Magnolfi F, Megna AS, Pretolani S, Regine R, Sponza M, Stasi R.
J Clin Oncol. 2009 Jun 1;27(16):2615-21
Percutaneous laser ablation of unresectable primary and metastatic adrenocortical carcinoma
Pacella CM, Stasi R, Bizzarri G, Pacella S, Graziano FM, Guglielmi R, Papini E.
Eur J Radiol. 2008 Apr; 66 (1):88-94
Complications of Laser Ablation for Hepatocellular Carcinoma: A Multicenter Study
Arienti V, Pretolani S, Pacella CM, Magnolfi F, Caspani B, Francica G, Megna AS, Regine R, Sponza M, Antico E, Di Lascio FM.
Radiology. 2008 Mar;246(3):947-55. Epub 2008 Jan 14.
Percutaneous laser ablation in patients with isolated unresectable liver metastases from colorectal cancer: Results of a phase II study.
Pacella CM, Valle D, Bizzarri G, Pacella S, Brunetti M, Maritati R, Osborn J, Stasi R.
Acta Oncologica 2006; 45: 77-83
Analysis of factors predicting survival in patients with hepatocellular carcinoma treated with percutaneous laser ablation.
Pacella CM, Bizzarri G, Francica G, Forlini G, Petrolati A, Valle D, Anelli V, Bianchini A, Nuntis SD, Pacella S, Rossi Z, Osborn J, Stasi R.
J Hepatol. 2006 Maggio;44(5):902-9
Percutaneous Laser Ablation in the Treatment of Hepatocellular Carcinoma with a Tumor Size of 4 cm or Smaller: Analysis of Factors Affecting the Achievement of Tumor Necrosis
Walser EM
J Vasc Interv Radiol 2005; 16:1427–1429
Laser Thermal Ablation in the Treatment of Small Hepatocellular Carcinoma: Results in 74 Patients
Pacella CM, Bizzarri G, Magnolfi F, Cecconi P, Caspani B, Anelli V, Bianchini A, Valle D, Pacella S, Manenti G, Rossi Z.
Radiology. 2001 Dec; 221(3):712-20.
Hepatocellular Carcinoma: Long-term Results of Combined Treatment with Laser Thermal Ablation and Transcatheter Arterial Chemoembolization
Pacella CM, Bizzarri G, Cecconi P, Caspani B, Magnolfi F, Bianchini A, Anelli V, Pacella S, Rossi Z.
Radiology. 2001 Jun;219(3):669-78
Ultrasound-guided percutaneous laser ablation of liver tissue in a rabbit model
Pacella CM, Rossi Z, Bizzarri G, Papini E, Marinozzi V, Paliotta D, Castaldo R, Ziparo V, Garosi F, Cinti M, Muzzi F
European Radiology 1993; 3(1)
Videos in the page are commented by GG di Costanzo, expert physician in liver lesion EchoLaser Therapy.
Radiofrequency Versus Laser Ablation for Hepatocellular Carcinoma
Randomised Clinical Trial
No. of patients enrolled: 140
Reference Study Centre: Cardarelli Hospital, Naples
Study Status: Completed
Registered on ClinicalTrial.gov: https://clinicaltrials.gov/ct2/show/NCT01096914?term=laser+radiofrequency+liver&rank=1
Publication of the results: Radiofrequency ablation versus laser ablation for the treatment of small hepatocellular carcinoma in cirrhosis: A randomized trial, Di Costanzo GG1, Tortora R, D’Adamo G, De Luca M, Lampasi F, Addario L, Galeota Lanza A, Picciotto FP, Tartaglione MT, Cordone G, Imparato M, Mattera S, Pacella CM. J Gastroenterol Hepatol. 2015 Mar;30(3):559-65.